Cholera
| Cholera | |
|---|---|
 | |
| A person with severe dehydration due to cholera causing sunken eyes and wrinkled hands and skin. | |
| Specialty | Infectious disease |
| Symptoms | Large amounts of watery diarrhea, vomiting, muscle cramps[1][2] |
| Complications | Dehydration, electrolyte imbalance[1] |
| Usual onset | 2 hours to 5 days after exposure[2] |
| Duration | Few days[1] |
| Causes | Vibrio cholerae spread by fecal-oral route[1][3] |
| Risk factors | Poor sanitation, not enough clean drinking water, poverty[1] |
| Diagnostic method | Stool test[1] |
| Prevention | Improved sanitation, clean water, cholera vaccines[1][4] |
| Treatment | Oral rehydration therapy, zinc supplementation, intravenous fluids, antibiotics[1][5] |
| Frequency | 3–5 million people a year[1] |
| Deaths | 28,800 (2015)[6] |
Cholera is an infection of the small intestine by some strains of the bacterium Vibrio cholerae.[3][2] Symptoms may range from none, to mild, to severe.[2] The classic symptom is large amounts of watery diarrhea that lasts a few days.[1]Vomiting and muscle cramps may also occur.[2] Diarrhea can be so severe that it leads within hours to severe dehydration and electrolyte imbalance.[1] This may result in sunken eyes, cold skin, decreased skin elasticity, and wrinkling of the hands and feet.[4] Dehydration can cause the skin to turn bluish.[7] Symptoms start two hours to five days after exposure.[2]
Cholera is caused by a number of types of Vibrio cholerae, with some types producing more severe disease than others.[1] It is spread mostly by unsafe water and unsafe food that has been contaminated with human feces containing the bacteria.[1] Undercooked seafood is a common source.[8] Humans are the only animal affected.[1]Risk factors for the disease include poor sanitation, not enough clean drinking water, and poverty.[1] There are concerns that rising sea levels will increase rates of disease.[1] Cholera can be diagnosed by a stool test.[1] A rapid dipstick test is available but is not as accurate.[9]
Prevention methods against cholera include improved sanitation and access to clean water.[4]Cholera vaccines that are given by mouth provide reasonable protection for about six months.[1] They have the added benefit of protecting against another type of diarrhea caused by E. coli.[1] The primary treatment is oral rehydration therapy—the replacement of fluids with slightly sweet and salty solutions.[1] Rice-based solutions are preferred.[1]Zinc supplementation is useful in children.[5] In severe cases, intravenous fluids, such as Ringer's lactate, may be required, and antibiotics may be beneficial.[1]Testing to see which antibiotic the cholera is susceptible to can help guide the choice.[2]
Cholera affects an estimated 3–5 million people worldwide and causes 28,800–130,000 deaths a year.[1][6] Although it is classified as a pandemic as of 2010[update], it is rare in the developed world.[1] Children are mostly affected.[1][10] Cholera occurs as both outbreaks and chronically in certain areas.[1] Areas with an ongoing risk of disease include Africa and Southeast Asia.[1] The risk of death among those affected is usually less than 5% but may be as high as 50%.[1] No access to treatment results in a higher death rate.[1] Descriptions of cholera are found as early as the 5th century BC in Sanskrit.[4] The study of cholera in England by John Snow between 1849 and 1854 led to significant advances in the field of epidemiology.[4][11]Seven large outbreaks have occurred over the last 200 years with millions of deaths.[12]
Contents
1 Signs and symptoms
2 Cause
2.1 Transmission
2.2 Susceptibility
3 Mechanism
3.1 Genetic structure
3.2 Antibiotic resistance
4 Diagnosis
5 Prevention
5.1 Surveillance
5.2 Vaccine
5.3 Sari filtration
6 Treatment
6.1 Fluids
6.2 Electrolytes
6.3 Antibiotics
6.4 Zinc supplementation
7 Prognosis
8 Epidemiology
9 History
10 Research
11 Society and culture
11.1 Health policy
11.2 Notable cases
12 References
13 External links
Signs and symptoms
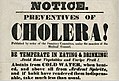
Typical cholera diarrhea that looks like "rice water".
The primary symptoms of cholera are profuse diarrhea and vomiting of clear fluid.[13] These symptoms usually start suddenly, half a day to five days after ingestion of the bacteria.[14] The diarrhea is frequently described as "rice water" in nature and may have a fishy odor.[13] An untreated person with cholera may produce 10 to 20 litres (3 to 5 US gal) of diarrhea a day.[13] Severe cholera, without treatment, kills about half of affected individuals.[13] If the severe diarrhea is not treated, it can result in life-threatening dehydration and electrolyte imbalances.[13] Estimates of the ratio of asymptomatic to symptomatic infections have ranged from 3 to 100.[15] Cholera has been nicknamed the "blue death"[16] because a person's skin may turn bluish-gray from extreme loss of fluids.[17]
Fever is rare and should raise suspicion for secondary infection. Patients can be lethargic, and might have sunken eyes, dry mouth, cold clammy skin, or wrinkled hands and feet. Kussmaul breathing, a deep and labored breathing pattern, can occur because of acidosis from stool bicarbonate losses and lactic acidosis associated with poor perfusion. Blood pressure drops due to dehydration, peripheral pulse is rapid and thready, and urine output decreases with time. Muscle cramping and weakness, altered consciousness, seizures, or even coma due to electrolyte imbalances are common, especially in children.[13]
Cause

Scanning electron microscope image of Vibrio cholerae

Vibrio cholerae, the bacterium that causes cholera.
Transmission
Cholera has been found in two animal populations: shellfish and plankton.[13]
Transmission is usually through the fecal-oral route of contaminated food or water caused by poor sanitation.[1] Most cholera cases in developed countries are a result of transmission by food, while in the developing world it is more often water.[13] Food transmission can occur when people harvest seafood such as oysters in waters infected with sewage, as Vibrio cholerae accumulates in planktonic crustaceans and the oysters eat the zooplankton.[18]
People infected with cholera often have diarrhea, and disease transmission may occur if this highly liquid stool, colloquially referred to as "rice-water", contaminates water used by others.[19] A single diarrheal event can cause a one-million fold increase in numbers of V. cholerae in the environment.[20] The source of the contamination is typically other cholera sufferers when their untreated diarrheal discharge is allowed to get into waterways, groundwater or drinking water supplies. Drinking any contaminated water and eating any foods washed in the water, as well as shellfish living in the affected waterway, can cause a person to contract an infection. Cholera is rarely spread directly from person to person.[medical citation needed]
V. cholerae also exists outside the human body in natural water sources, either by itself or through interacting with phytoplankton, zooplankton, or biotic and abiotic detritus.[21] Drinking such water can also result in the disease, even without prior contamination through fecal matter. Selective pressures exist however in the aquatic environment that may reduce the virulence of V. cholerae.[21] Specifically, animal models indicate that the transcriptional profile of the pathogen changes as it prepares to enter an aquatic environment.[21] This transcriptional change results in a loss of ability of V. cholerae to be cultured on standard media, a phenotype referred to as 'viable but non-culturable' (VBNC) or more conservatively 'active but non-culturable' (ABNC).[21] One study indicates that the culturability of V. cholerae drops 90% within 24 hours of entering the water, and furthermore that this loss in culturability is associated with a loss in virulence.[21][22]
Both toxic and non-toxic strains exist. Non-toxic strains can acquire toxicity through a temperate bacteriophage.[23]
Susceptibility
About 100 million bacteria must typically be ingested to cause cholera in a normal healthy adult.[13] This dose, however, is less in those with lowered gastric acidity (for instance those using proton pump inhibitors).[13] Children are also more susceptible, with two- to four-year-olds having the highest rates of infection.[13] Individuals' susceptibility to cholera is also affected by their blood type, with those with type O blood being the most susceptible.[13] Persons with lowered immunity, such as persons with AIDS or malnourished children, are more likely to experience a severe case if they become infected.[24] Any individual, even a healthy adult in middle age, can experience a severe case, and each person's case should be measured by the loss of fluids, preferably in consultation with a professional health care provider.[medical citation needed]
The cystic fibrosis genetic mutation known as delta-F508 in humans has been said to maintain a selective heterozygous advantage: heterozygous carriers of the mutation (who are thus not affected by cystic fibrosis) are more resistant to V. cholerae infections.[25] In this model, the genetic deficiency in the cystic fibrosis transmembrane conductance regulator channel proteins interferes with bacteria binding to the intestinal epithelium, thus reducing the effects of an infection.
Mechanism

The role of biofilm in the intestinal colonization of Vibrio cholerae.
When consumed, most bacteria do not survive the acidic conditions of the human stomach.[26] The few surviving bacteria conserve their energy and stored nutrients during the passage through the stomach by shutting down protein production. When the surviving bacteria exit the stomach and reach the small intestine, they must propel themselves through the thick mucus that lines the small intestine to reach the intestinal walls where they can attach and thrive.[26]
Once the cholera bacteria reach the intestinal wall, they no longer need the flagella to move. The bacteria stop producing the protein flagellin to conserve energy and nutrients by changing the mix of proteins which they express in response to the changed chemical surroundings. On reaching the intestinal wall, V. cholerae start producing the toxic proteins that give the infected person a watery diarrhea. This carries the multiplying new generations of V. cholerae bacteria out into the drinking water of the next host if proper sanitation measures are not in place.[medical citation needed]
The cholera toxin (CTX or CT) is an oligomeric complex made up of six protein subunits: a single copy of the A subunit (part A), and five copies of the B subunit (part B), connected by a disulfide bond. The five B subunits form a five-membered ring that binds to GM1 gangliosides on the surface of the intestinal epithelium cells. The A1 portion of the A subunit is an enzyme that ADP-ribosylates G proteins, while the A2 chain fits into the central pore of the B subunit ring. Upon binding, the complex is taken into the cell via receptor-mediated endocytosis. Once inside the cell, the disulfide bond is reduced, and the A1 subunit is freed to bind with a human partner protein called ADP-ribosylation factor 6 (Arf6).[27] Binding exposes its active site, allowing it to permanently ribosylate the Gs alpha subunit of the heterotrimeric G protein. This results in constitutive cAMP production, which in turn leads to the secretion of water, sodium, potassium, and bicarbonate into the lumen of the small intestine and rapid dehydration. The gene encoding the cholera toxin was introduced into V. cholerae by horizontal gene transfer. Virulent strains of V. cholerae carry a variant of a temperate bacteriophage called CTXφ.
Microbiologists have studied the genetic mechanisms by which the V. cholerae bacteria turn off the production of some proteins and turn on the production of other proteins as they respond to the series of chemical environments they encounter, passing through the stomach, through the mucous layer of the small intestine, and on to the intestinal wall.[28] Of particular interest have been the genetic mechanisms by which cholera bacteria turn on the protein production of the toxins that interact with host cell mechanisms to pump chloride ions into the small intestine, creating an ionic pressure which prevents sodium ions from entering the cell. The chloride and sodium ions create a salt-water environment in the small intestines, which through osmosis can pull up to six liters of water per day through the intestinal cells, creating the massive amounts of diarrhea. The host can become rapidly dehydrated unless an appropriate mixture of dilute salt water and sugar is taken to replace the blood's water and salts lost in the diarrhea.[medical citation needed]
By inserting separate, successive sections of V. cholerae DNA into the DNA of other bacteria, such as E. coli that would not naturally produce the protein toxins, researchers have investigated the mechanisms by which V. cholerae responds to the changing chemical environments of the stomach, mucous layers, and intestinal wall. Researchers have discovered a complex cascade of regulatory proteins controls expression of V. cholerae virulence determinants.[medical citation needed] In responding to the chemical environment at the intestinal wall, the V. cholerae bacteria produce the TcpP/TcpH proteins, which, together with the ToxR/ToxS proteins, activate the expression of the ToxT regulatory protein. ToxT then directly activates expression of virulence genes that produce the toxins, causing diarrhea in the infected person and allowing the bacteria to colonize the intestine.[28] Current[when?] research aims at discovering "the signal that makes the cholera bacteria stop swimming and start to colonize (that is, adhere to the cells of) the small intestine."[28]
Genetic structure
Amplified fragment length polymorphism fingerprinting of the pandemic isolates of V. cholerae has revealed variation in the genetic structure. Two clusters have been identified: Cluster I and Cluster II. For the most part, Cluster I consists of strains from the 1960s and 1970s, while Cluster II largely contains strains from the 1980s and 1990s, based on the change in the clone structure. This grouping of strains is best seen in the strains from the African continent.[29]
Antibiotic resistance
In many areas of the world, antibiotic resistance is increasing within cholera bacteria. In Bangladesh, for example, most cases are resistant to tetracycline, trimethoprim-sulfamethoxazole, and erythromycin.[30] Rapid diagnostic assay methods are available for the identification of multi-drug resistant cases.[31] New generation antimicrobials have been discovered which are effective against cholera bacteria in in vitro studies.[32]
Diagnosis
A rapid dipstick test is available to determine the presence of V. cholerae.[30] In those samples that test positive, further testing should be done to determine antibiotic resistance.[30] In epidemic situations, a clinical diagnosis may be made by taking a patient history and doing a brief examination. Treatment is usually started without or before confirmation by laboratory analysis.
Stool and swab samples collected in the acute stage of the disease, before antibiotics have been administered, are the most useful specimens for laboratory diagnosis. If an epidemic of cholera is suspected, the most common causative agent is V. cholerae O1. If V. cholerae serogroup O1 is not isolated, the laboratory should test for V. cholerae O139. However, if neither of these organisms is isolated, it is necessary to send stool specimens to a reference laboratory.
Infection with V. cholerae O139 should be reported and handled in the same manner as that caused by V. cholerae O1. The associated diarrheal illness should be referred to as cholera and must be reported in the United States.[33]
Prevention

Preventive inoculation against cholera in 1966.
The World Health Organization (WHO) recommends focusing on prevention, preparedness, and response to combat the spread of cholera.[34] They also stress the importance of an effective surveillance system.[34] Governments can play a role in all of these areas.
Although cholera may be life-threatening, prevention of the disease is normally straightforward if proper sanitation practices are followed. In developed countries, due to nearly universal advanced water treatment and sanitation practices present there, cholera is rare. For example, the last major outbreak of cholera in the United States occurred in 1910–1911.[35][36] Cholera is mainly a risk in developing countries.
Effective sanitation practices, if instituted and adhered to in time, are usually sufficient to stop an epidemic. There are several points along the cholera transmission path at which its spread may be halted:[citation needed]
- Sterilization: Proper disposal and treatment of all materials that may have come into contact with cholera victims' feces (e.g., clothing, bedding, etc.) are essential. These should be sanitized by washing in hot water, using chlorine bleach if possible. Hands that touch cholera patients or their clothing, bedding, etc., should be thoroughly cleaned and disinfected with chlorinated water or other effective antimicrobial agents.
Sewage and fecal sludge management: In cholera-affected areas, sewage and fecal sludge need to be treated and managed carefully in order to stop the spread of this disease via human excreta. Provision of sanitation and hygiene is an important preventative measure.[34]Open defecation, release of untreated sewage, or dumping of fecal sludge from pit latrines or septic tanks into the environment need to be prevented.[37] In many cholera affected zones, there is a low degree of sewage treatment.[38][39] Therefore, the implementation of dry toilets that do not contribute to water pollution, as they do not flush with water, may be an interesting alternative to flush toilets.[40]
- Sources: Warnings about possible cholera contamination should be posted around contaminated water sources with directions on how to decontaminate the water (boiling, chlorination etc.) for possible use.
Water purification: All water used for drinking, washing, or cooking should be sterilized by either boiling, chlorination, ozone water treatment, ultraviolet light sterilization (e.g., by solar water disinfection), or antimicrobial filtration in any area where cholera may be present. Chlorination and boiling are often the least expensive and most effective means of halting transmission. Cloth filters or sari filtration, though very basic, have significantly reduced the occurrence of cholera when used in poor villages in Bangladesh that rely on untreated surface water. Better antimicrobial filters, like those present in advanced individual water treatment hiking kits, are most effective. Public health education and adherence to appropriate sanitation practices are of primary importance to help prevent and control transmission of cholera and other diseases.
Handwashing with soap or ash after using a toilet and before handling food or eating is also recommended for cholera prevention by WHO Africa.[41]

Dumping of sewage or fecal sludge from a UN camp into a lake in the surroundings of Port-au-Prince is thought to have contributed to the spread of cholera after the Haiti earthquake in 2010, killing thousands.

Example of a urine-diverting dry toilet in a cholera-affected area in Haiti. This type of toilet stops transmission of disease via the fecal-oral route due to water pollution.

Cholera hospital in Dhaka, showing typical "cholera beds".
Surveillance
 Play media
Play mediaA modelling approach using satellite data can enhance our ability to develop cholera risk maps in several regions of the globe.
Surveillance and prompt reporting allow for containing cholera epidemics rapidly. Cholera exists as a seasonal disease in many endemic countries, occurring annually mostly during rainy seasons. Surveillance systems can provide early alerts to outbreaks, therefore leading to coordinated response and assist in preparation of preparedness plans. Efficient surveillance systems can also improve the risk assessment for potential cholera outbreaks. Understanding the seasonality and location of outbreaks provides guidance for improving cholera control activities for the most vulnerable.[42] For prevention to be effective, it is important that cases be reported to national health authorities.[13]
Vaccine
A number of safe and effective oral vaccines for cholera are available.[43] The World Health Organization has three prequalified oral cholera vaccines (OCVs): Dukoral, Sanchol, and Euvichol. Dukoral, an orally administered, inactivated whole cell vaccine, has an overall efficacy of about 52% during the first year after being given and 62% in the second year, with minimal side effects.[43] It is available in over 60 countries. However, it is not currently[when?] recommended by the Centers for Disease Control and Prevention (CDC) for most people traveling from the United States to endemic countries.[44] The vaccine that the FDA recommends, Vaxchora, is an oral attenuated live vaccine, that is effective as a single dose.[45]
One injectable vaccine was found to be effective for two to three years. The protective efficacy was 28% lower in children less than 5 years old.[46] However, as of 2010[update], it has limited availability.[1] Work is under way to investigate the role of mass vaccination.[47] The World Health Organization (WHO) recommends immunization of high-risk groups, such as children and people with HIV, in countries where this disease is endemic.[1] If people are immunized broadly, herd immunity results, with a decrease in the amount of contamination in the environment.[30]
Sari filtration
An effective and relatively cheap method to prevent the transmission of cholera is the use of a folded sari (a long cloth garment) to filter drinking water.[48] In Bangladesh this practice was found to decrease rates of cholera by nearly half.[49] It involves folding a sari four to eight times.[48] Between uses the cloth should be rinsed in clean water and dried in the sun to kill any bacteria on it.[50] A nylon cloth appears to work as well but is not as affordable.[49]
Treatment

Cholera patient being treated by oral rehydration therapy in 1992.
Continued eating speeds the recovery of normal intestinal function. The World Health Organization recommends this generally for cases of diarrhea no matter what the underlying cause.[51] A CDC training manual specifically for cholera states: "Continue to breastfeed your baby if the baby has watery diarrhea, even when traveling to get treatment. Adults and older children should continue to eat frequently."[52]
Fluids
The most common error in caring for patients with cholera is to underestimate the speed
and volume of fluids required.[53] In most cases, cholera can be successfully treated with oral rehydration therapy (ORT), which is highly effective, safe, and simple to administer.[30] Rice-based solutions are preferred to glucose-based ones due to greater efficiency.[30] In severe cases with significant dehydration, intravenous rehydration may be necessary. Ringer's lactate is the preferred solution, often with added potassium.[13][51] Large volumes and continued replacement until diarrhea has subsided may be needed.[13] Ten percent of a person's body weight in fluid may need to be given in the first two to four hours.[13] This method was first tried on a mass scale during the Bangladesh Liberation War, and was found to have much success.[54] Despite widespread beliefs, fruit juices and commercial fizzy drinks like cola, are not ideal for rehydration of people with serious infections of the intestines, and their excessive sugar content may even harm water uptake.[55]
If commercially produced oral rehydration solutions are too expensive or difficult to obtain, solutions can be made. One such recipe calls for 1 liter of boiled water, 1/2 teaspoon of salt, 6 teaspoons of sugar, and added mashed banana for potassium and to improve taste.[56]
Electrolytes
As there frequently is initially acidosis, the potassium level may be normal, even though large losses have occurred.[13] As the dehydration is corrected, potassium levels may decrease rapidly, and thus need to be replaced.[13] This may be done by consuming foods high in potassium, like bananas or coconut water.[57]
Antibiotics
Antibiotic treatments for one to three days shorten the course of the disease and reduce the severity of the symptoms.[13] Use of antibiotics also reduces fluid requirements.[58] People will recover without them, however, if sufficient hydration is maintained.[30] The World Health Organization only recommends antibiotics in those with severe dehydration.[57]
Doxycycline is typically used first line, although some strains of V. cholerae have shown resistance.[13] Testing for resistance during an outbreak can help determine appropriate future choices.[13] Other antibiotics proven to be effective include cotrimoxazole, erythromycin, tetracycline, chloramphenicol, and furazolidone.[59]Fluoroquinolones, such as ciprofloxacin, also may be used, but resistance has been reported.[60]
Antibiotics improve outcomes in those who are both severely and not severely dehydrated.[61]Azithromycin and tetracycline may work better than doxycycline or ciprofloxacin.[61]
Zinc supplementation
In Bangladesh zinc supplementation reduced the duration and severity of diarrhea in children with cholera when given with antibiotics and rehydration therapy as needed. It reduced the length of disease by eight hours and the amount of diarrhea stool by 10%.[62] Supplementation appears to be also effective in both treating and preventing infectious diarrhea due to other causes among children in the developing world.[62][63]
Prognosis
If people with cholera are treated quickly and properly, the mortality rate is less than 1%; however, with untreated cholera, the mortality rate rises to 50–60%.[13][64]
For certain genetic strains of cholera, such as the one present during the 2010 epidemic in Haiti and the 2004 outbreak in India, death can occur within two hours of becoming ill.[65]
Epidemiology
Cholera affects an estimated 3–5 million people worldwide, and causes 58,000–130,000 deaths a year as of 2010[update].[1][66] This occurs mainly in the developing world.[67] In the early 1980s, death rates are believed to have been greater than three million a year.[13] It is difficult to calculate exact numbers of cases, as many go unreported due to concerns that an outbreak may have a negative impact on the tourism of a country.[30] Cholera remains[when?] both epidemic and endemic in many areas of the world.[13] In October 2016, an outbreak of cholera began in war-ravaged Yemen.[68] WHO called it "the worst cholera outbreak in the world".[69]
Although much is known about the mechanisms behind the spread of cholera, this has not led to a full understanding of what makes cholera outbreaks happen in some places and not others. Lack of treatment of human feces and lack of treatment of drinking water greatly facilitate its spread, but bodies of water can serve as a reservoir, and seafood shipped long distances can spread the disease. Cholera was not known in the Americas for most of the 20th century, but it reappeared towards the end of that century.[70]
History

Map of the 2008–2009 cholera outbreak in sub-Saharan Africa showing the statistics as of 12 February 2009.
The word cholera is from Greek: χολέρα kholera from χολή kholē "bile". Cholera likely has its origins in the Indian subcontinent as evidenced by its prevalence in the region for centuries.[13] Early outbreaks in the Indian subcontinent are believed to have been the result of poor living conditions as well as the presence of pools of still water, both of which provide ideal conditions for cholera to thrive.[71] The disease first spread by trade routes (land and sea) to Russia in 1817, later to the rest of Europe, and from Europe to North America and the rest of the world.[13] Seven cholera pandemics have occurred in the past 200 years, with the seventh pandemic originating in Indonesia in 1961.[72]
The first cholera pandemic occurred in the Bengal region of India, near Calcutta starting in 1817 through 1824. The disease dispersed from India to Southeast Asia, the Middle East, Europe, and Eastern Africa.[73] The movement of British Army and Navy ships and personnel is believed to have contributed to the range of the pandemic, since the ships carried people with the disease to the shores of the Indian Ocean, from Africa to Indonesia, and north to China and Japan.[74] The second pandemic lasted from 1826 to 1837 and particularly affected North America and Europe due to the result of advancements in transportation and global trade, and increased human migration, including soldiers.[75] The third pandemic erupted in 1846, persisted until 1860, extended to North Africa, and reached South America, for the first time specifically affecting Brazil. The fourth pandemic lasted from 1863 to 1875 spread from India to Naples and Spain. The fifth pandemic was from 1881–1896 and started in India and spread to Europe, Asia, and South America. The sixth pandemic started 1899–1923. These epidemics were less fatal due to a greater understanding of the cholera bacteria. Egypt, the Arabian peninsula, Persia, India, and the Philippines were hit hardest during these epidemics, while other areas, like Germany in 1892 and Naples from 1910–1911, also experienced severe outbreaks. The seventh pandemic originated in 1961 in Indonesia and is marked by the emergence of a new strain, nicknamed El Tor, which still persists (as of 2018[update][76]) in developing countries.[77]
Since it became widespread in the 19th century, cholera has killed tens of millions of people.[78] In Russia alone, between 1847 and 1851, more than one million people perished of the disease.[79] It killed 150,000 Americans during the second pandemic.[80] Between 1900 and 1920, perhaps eight million people died of cholera in India.[81] Cholera became the first reportable disease in the United States due to the significant effects it had on health.[13]John Snow, in England, was the first to identify the importance of contaminated water as its cause in 1854.[13] Cholera is now no longer considered a pressing health threat in Europe and North America due to filtering and chlorination of water supplies, but still heavily affects populations in developing countries.
In the past, vessels flew a yellow quarantine flag if any crew members or passengers were suffering from cholera. No one aboard a vessel flying a yellow flag would be allowed ashore for an extended period, typically 30 to 40 days.[82] In modern[when?] sets of international maritime signal flags, the quarantine flag is yellow and black.
Historically many different claimed remedies have existed in folklore. Many of the older remedies were based on the miasma theory. Some believed that abdominal chilling made one more susceptible and flannel and cholera belts were routine in army kits.[83] In the 1854–1855 outbreak in Naples homeopathic camphor was used according to Hahnemann.[84] T. J. Ritter's "Mother's Remedies" book lists tomato syrup as a home remedy from northern America. Elecampane was recommended in the United Kingdom according to William Thomas Fernie.[85]
Cholera cases are much less frequent in developed countries where governments have helped to establish water sanitation practices and effective medical treatments.[86] The United States, for example, used to[when?] have a severe cholera problem similar to those in some developing countries. There were three large cholera outbreaks in the 1800s, which can be attributed to Vibrio cholerae's spread through interior waterways like the Erie Canal and routes along the Eastern Seaboard.[87] The island of Manhattan in New York City touched the Atlantic Ocean, where cholera collected just off the coast. At this time, New York City did not have as effective a sanitation system as it does today,[when?] so cholera was able to spread.[88]
Cholera morbus is a historical term that was used to refer to gastroenteritis rather than specifically cholera.[89]

Drawing of Death bringing cholera, in Le Petit Journal (1912).
Emperor Pedro II of Brazil visiting people with cholera in 1855.
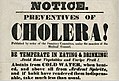
Hand bill from the New York City Board of Health, 1832—the outdated public health advice demonstrates the lack of understanding of the disease and its actual causative factors.
Signal flag "Lima" called the "Yellow Jack" which when flown in harbor means ship is under quarantine.
Research

Robert Koch (third from the right) on a cholera research expedition in Egypt in 1884, one year after he identified V. cholerae.

How to avoid the cholera leaflet; Aberystwyth; August 1849.
The bacterium was isolated in 1854 by Italian anatomist Filippo Pacini,[90] but its exact nature and his results were not widely known.
Spanish physician Jaume Ferran i Clua developed a cholera inoculation in 1885, the first to immunize humans against a bacterial disease.[91]
Russian-Jewish bacteriologist Waldemar Haffkine developed the first cholera vaccine in July 1892.[92]
One of the major contributions to fighting cholera was made by the physician and pioneer medical scientist John Snow (1813–1858), who in 1854 found a link between cholera and contaminated drinking water.[71] Dr. Snow proposed a microbial origin for epidemic cholera in 1849. In his major "state of the art" review of 1855, he proposed a substantially complete and correct model for the cause of the disease. In two pioneering epidemiological field studies, he was able to demonstrate human sewage contamination was the most probable disease vector in two major epidemics in London in 1854.[93] His model was not immediately accepted, but it was seen to be the more plausible, as medical microbiology developed over the next 30 years or so.
Cities in developed nations made massive investment in clean water supply and well-separated sewage treatment infrastructures between the mid-1850s and the 1900s. This eliminated the threat of cholera epidemics from the major developed cities in the world. In 1883, Robert Koch identified V. cholerae with a microscope as the bacillus causing the disease.[94]
Robert Allan Phillips, working at the US Naval Medical Research Unit Two in Southeast Asia, evaluated the pathophysiology of the disease using modern laboratory chemistry techniques and developed a protocol for rehydration. His research led the Lasker Foundation to award him its prize in 1967.[95]
More recently, in 2002, Alam, et al., studied stool samples from patients at the International Centre for Diarrhoeal Disease in Dhaka, Bangladesh. From the various experiments they conducted, the researchers found a correlation between the passage of V. cholerae through the human digestive system and an increased infectivity state. Furthermore, the researchers found the bacterium creates a hyperinfected state where genes that control biosynthesis of amino acids, iron uptake systems, and formation of periplasmic nitrate reductase complexes were induced just before defecation. These induced characteristics allow the cholera vibrios to survive in the "rice water" stools, an environment of limited oxygen and iron, of patients with a cholera infection.[96]
Society and culture
Health policy
In many developing countries, cholera still reaches its victims through contaminated water sources, and countries without proper sanitation techniques have greater incidence of the disease.[97] Governments can play a role in this. In 2008, for example, the Zimbabwean cholera outbreak was due partly to the government's role, according to a report from the James Baker Institute.[18] The Haitian government's inability to provide safe drinking water after the 2010 earthquake led to an increase in cholera cases as well.[98]
Similarly, South Africa's cholera outbreak was exacerbated by the government's policy of privatizing water programs. The wealthy elite of the country were able to afford safe water while others had to use water from cholera-infected rivers.[not in citation given][99]
According to Rita R. Colwell of the James Baker Institute, if cholera does begin to spread, government preparedness is crucial. A government's ability to contain the disease before it extends to other areas can prevent a high death toll and the development of an epidemic or even pandemic. Effective disease surveillance can ensure that cholera outbreaks are recognized as soon as possible and dealt with appropriately. Oftentimes, this will allow public health programs to determine and control the cause of the cases, whether it is unsanitary water or seafood that have accumulated a lot of Vibrio cholerae specimens.[18] Having an effective surveillance program contributes to a government's ability to prevent cholera from spreading. In the year 2000 in the state of Kerala in India, the Kottayam district was determined to be "Cholera-affected"; this pronouncement led to task forces that concentrated on educating citizens with 13,670 information sessions about human health.[100] These task forces promoted the boiling of water to obtain safe water, and provided chlorine and oral rehydration salts.[100] Ultimately, this helped to control the spread of the disease to other areas and minimize deaths. On the other hand, researchers have shown that most of the citizens infected during the 1991 cholera outbreak in Bangladesh lived in rural areas, and were not recognized by the government's surveillance program. This inhibited physicians' abilities to detect cholera cases early.[101]
According to Colwell, the quality and inclusiveness of a country's health care system affects the control of cholera, as it did in the Zimbabwean cholera outbreak.[18] While sanitation practices are important, when governments respond quickly and have readily available vaccines, the country will have a lower cholera death toll. Affordability of vaccines can be a problem; if the governments do not provide vaccinations, only the wealthy may be able to afford them and there will be a greater toll on the country's poor.[102][103] The speed with which government leaders respond to cholera outbreaks is important.[104]
Besides contributing to an effective or declining public health care system and water sanitation treatments, government can have indirect effects on cholera control and the effectiveness of a response to cholera.[105] A country's government can impact its ability to prevent disease and control its spread. A speedy government response backed by a fully functioning health care system and financial resources can prevent cholera's spread. This limits cholera's ability to cause death, or at the very least a decline in education, as children are kept out of school to minimize the risk of infection.[105]
Notable cases
Tchaikovsky's death has traditionally been attributed to cholera, most probably contracted through drinking contaminated water several days earlier.[106] Tchaikovsky's mother died of cholera,[107] and his father became sick with cholera at this time but made a full recovery.[108] Some scholars, however, including English musicologist and Tchaikovsky authority David Brown and biographer Anthony Holden, have theorized that his death was a suicide.[109]
2010 Haiti cholera outbreak. Ten months after the 2010 earthquake, an outbreak swept over Haiti, traced to a United Nations base of peacekeepers from Nepal.[110] This marks the worst cholera outbreak in recent history, as well as the best documented cholera outbreak in modern public health.
Sadi Carnot, Physicist, a founder of thermodynamics (d. 1832)[111]
Charles X, King of France (d. 1836)[112]
James K. Polk, eleventh president of the United States (d. 1849)[113]
Carl von Clausewitz, Prussian soldier and German military theorist (d. 1831)[114]
Elliot Bovill, Chief Justice of the Straits Settlements (1893)[115]
References
^ abcdefghijklmnopqrstuvwxyzaaabacadaeafag "Cholera vaccines: WHO position paper" (PDF). Wkly. Epidemiol. Rec. 85 (13): 117–128. March 26, 2010. PMID 20349546. Archived (PDF) from the original on April 13, 2015..mw-parser-output cite.citation{font-style:inherit}.mw-parser-output q{quotes:"""""""'""'"}.mw-parser-output code.cs1-code{color:inherit;background:inherit;border:inherit;padding:inherit}.mw-parser-output .cs1-lock-free a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-subscription a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration{color:#555}.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration span{border-bottom:1px dotted;cursor:help}.mw-parser-output .cs1-hidden-error{display:none;font-size:100%}.mw-parser-output .cs1-visible-error{font-size:100%}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-format{font-size:95%}.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-left{padding-left:0.2em}.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-right{padding-right:0.2em}
^ abcdefg "Cholera – Vibrio cholerae infection Information for Public Health & Medical Professionals". Centers for Disease Control and Prevention. January 6, 2015. Archived from the original on 20 March 2015. Retrieved 17 March 2015.
^ ab Finkelstein, Richard. "Medical microbiology". Archived from the original on 1 September 2017. Retrieved 14 August 2016.
^ abcde Harris, JB; LaRocque, RC; Qadri, F; Ryan, ET; Calderwood, SB (30 June 2012). "Cholera". Lancet. 379 (9835): 2466–76. doi:10.1016/s0140-6736(12)60436-x. PMC 3761070. PMID 22748592.
^ ab "Cholera – Vibrio cholerae infection Treatment". Centers for Disease Control and Prevention. November 7, 2014. Archived from the original on 11 March 2015. Retrieved 17 March 2015.
^ ab GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
^ Bailey, Diane (2011). Cholera (1st ed.). New York: Rosen Pub. p. 7. ISBN 978-1-4358-9437-2. Archived from the original on 2016-12-03.
^ "Sources of Infection & Risk Factors". Centers for Disease Control and Prevention. November 7, 2014. Archived from the original on 12 March 2015. Retrieved 17 March 2015.
^ "Diagnosis and Detection". Centers for Disease Control and Prevention. February 10, 2015. Archived from the original on 15 March 2015. Retrieved 17 March 2015.
^ "Cholera – Vibrio cholerae infection". Centers for Disease Control and Prevention. October 27, 2014. Archived from the original on 17 March 2015. Retrieved 17 March 2015.
^ Timmreck, Thomas C. (2002). An introduction to epidemiology (3. ed.). Sudbury, MA: Jones and Bartlett Publishers. p. 77. ISBN 978-0-7637-0060-7. Archived from the original on 2016-12-03.
^ "Cholera's seven pandemics". CBC. 9 May 2008. Retrieved 15 July 2018.
^ abcdefghijklmnopqrstuvwxyzaaab Sack DA, Sack RB, Nair GB, Siddique AK (January 2004). "Cholera". Lancet. 363 (9404): 223–33. doi:10.1016/S0140-6736(03)15328-7. PMID 14738797.
^ Azman AS, Rudolph KE, Cummings DA, Lessler J (November 2012). "The incubation period of cholera: A systematic review". J. Infect. 66 (5): 432–438. doi:10.1016/j.jinf.2012.11.013. PMC 3677557. PMID 23201968.
^ King AA, Ionides EL, Pascual M, Bouma MJ (August 2008). "Inapparent infections and cholera dynamics" (PDF). Nature. 454 (7206): 877–80. Bibcode:2008Natur.454..877K. doi:10.1038/nature07084. PMID 18704085.
^ Greenough, William B. (2 January 2008). "The blue death Disease, disaster, and the water we drink". The Journal of Clinical Investigation. 118 (1): 4. doi:10.1172/JCI34394. PMC 2171164.
^ McElroy, Ann; Townsend, Patricia K. (2009). Medical Anthropology in Ecological Perspective. Boulder, CO: Westview. p. 375. ISBN 978-0-8133-4384-6.
^ abcd Rita Colwell. Oceans, Climate, and Health: Cholera as a Model of Infectious Diseases in a Changing Environment. Rice University: James A Baker III Institute for Public Policy. Archived from the original on 2013-10-26. Retrieved 2013-10-23.
^ Ryan KJ; Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 376–7. ISBN 978-0-8385-8529-0.
^ "Cholera Biology and Genetics | NIH: National Institute of Allergy and Infectious Diseases". www.niaid.nih.gov. Retrieved 2017-12-05.
^ abcde Nelson, EJ; Harris, JB; Morris, JG; Calderwood, SB; Camilli, A (7 October 2009). "Cholera transmission: the host, pathogen and bacteriophage dynamic". Nat Rev Microbiol. 7 (10): 693–702. doi:10.1038/nrmicro2204. PMC 3842031. PMID 19756008.
^ Nelson, EJ; Chowdhury, A; Flynn, J; Schild, Stefan; Bourassa, L; Shao, Yue; LaRocque, RC; Calderwood, SB; Qadri, F; Camilli, A (24 October 2008). "Transmission of Vibrio cholerae Is Antagonized by Lytic Phage and Entry into the Aquatic Environment". PLoS Pathog. 4 (10): e1000187. doi:10.1371/journal.ppat.1000187. PMC 2563029. PMID 18949027.
^ Archivist (1997). "Cholera phage discovery". Arch. Dis. Child. 76 (3): 274. doi:10.1136/adc.76.3.274. PMC 1717096. Archived from the original on 2008-12-16.
^ Prevention and control of cholera outbreaks: WHO policy and recommendations Archived 2011-11-22 at the Wayback Machine., World Health Organization, Regional Office for the Eastern Mediterranean, undated but citing sources from '07, '04, '03, '04, and '05.
^ Bertranpetit J, Calafell F (1996). "Genetic and geographical variability in cystic fibrosis: evolutionary considerations". Ciba Found. Symp. 197: 97–114, discussion 114–8. PMID 8827370.
^ ab Almagro-Moreno, S; Pruss, K; Taylor, RK (May 2015). "Intestinal Colonization Dynamics of Vibrio cholerae". PLOS Pathog. 11 (5): e1004787. doi:10.1371/journal.ppat.1004787. PMC 4440752. PMID 25996593.
^ O'Neal CJ, Jobling MG, Holmes RK, Hol WG (2005). "Structural basis for the activation of cholera toxin by human ARF6-GTP". Science. 309 (5737): 1093–6. Bibcode:2005Sci...309.1093O. doi:10.1126/science.1113398. PMID 16099990.
^ abc DiRita VJ, Parsot C, Jander G, Mekalanos JJ (June 1991). "Regulatory cascade controls virulence in Vibrio cholerae". Proc. Natl. Acad. Sci. U.S.A. 88 (12): 5403–7. Bibcode:1991PNAS...88.5403D. doi:10.1073/pnas.88.12.5403. PMC 51881. PMID 2052618.
^ [unreliable medical source?]Lan R, Reeves PR (January 2002). "Pandemic Spread of Cholera: Genetic Diversity and Relationships within the Seventh Pandemic Clone of Vibrio cholerae Determined by Amplified Fragment Length Polymorphism". J. Clin. Microbiol. 40 (1): 172–181. doi:10.1128/JCM.40.1.172-181.2002. ISSN 0095-1137. PMC 120103. PMID 11773113.
^ abcdefgh Sack DA, Sack RB, Chaignat CL (August 2006). "Getting serious about cholera". N. Engl. J. Med. 355 (7): 649–51. doi:10.1056/NEJMp068144. PMID 16914700.
^ Mackay IM, ed. (2007). Real-Time PCR in microbiology: From diagnosis to characterization. Caister Academic Press. ISBN 978-1-904455-18-9.
^ Ramamurthy T (2008). "Antibiotic resistance in Vibrio cholerae". Vibrio cholerae: Genomics and molecular biology. Caister Academic Press. ISBN 978-1-904455-33-2.
^ "Laboratory Methods for the Diagnosis of Epidemic Dysentery and Cholera" (PDF). Centers for Disease Control and Prevention. 1999. Archived (PDF) from the original on 2017-06-23. Retrieved 2017-06-30.
^ abc "Cholera Fact Sheet", World Health Organization. who.int Archived 2012-05-05 at the Wayback Machine.. Retrieved November 5, 2013.
^ "Cholera Kills Boy. All Other Suspected Cases Now in Quarantine and Show No Alarming Symptoms" (PDF). The New York Times. July 18, 1911. Retrieved 2008-07-28.The sixth death from cholera since the arrival in this port from Naples of the steamship Moltke, thirteen days ago, occurred yesterday at Swineburne Island. The victim was Francesco Farando, 14 years old.
[dead link]
^ "More Cholera in Port". Washington Post. October 10, 1910. Archived from the original on December 16, 2008. Retrieved 2008-12-11.A case of cholera developed today in the steerage of the Hamburg-American liner Moltke, which has been detained at quarantine as a possible cholera carrier since Monday last. Dr. A.H. Doty, health officer of the port, reported the case tonight with the additional information that another cholera patient from the Moltke is under treatment at Swinburne Island.
^ Cisneros, Blanca Jimenez; Rose, Joan B. (2009-03-24). Urban Water Security: Managing Risks: UNESCO-IHP. CRC Press. ISBN 978-0-203-88162-0.
^ Drasar, B. S.; Forrest, B. D. (2012-12-06). Cholera and the Ecology of Vibrio cholerae. Springer Science & Business Media. p. 24. ISBN 978-94-009-1515-2.
^ Singer, Merrill (2016-05-31). A Companion to the Anthropology of Environmental Health. John Wiley & Sons. p. 219. ISBN 978-1-118-78699-4.
^ (www.dw.com), Deutsche Welle. "Starting a poop to compost movement | Global Ideas | DW | 09.06.2015". DW.COM. Retrieved 2017-10-01.
^ "Cholera and food safety" (PDF). World Health Organization. Archived (PDF) from the original on 2017-08-21. Retrieved 2017-08-20.
^ "Cholera: prevention and control". Health topics. WHO. 2008. Archived from the original on 2008-12-14. Retrieved 2008-12-08.
^ ab Sinclair D, Abba K, Zaman K, Qadri F, Graves PM (2011). Sinclair D, ed. "Oral vaccines for preventing cholera". Cochrane Database Syst. Rev. (3): CD008603. doi:10.1002/14651858.CD008603.pub2. PMID 21412922.
^ "Is a vaccine available to prevent cholera?". CDC disease info: Cholera. 2010-10-22. Archived from the original on 2010-10-26. Retrieved 2010-10-24.
^ FDA Product Approval – Immunization Action Coalition Archived 2017-04-15 at the Wayback Machine.
^ Graves PM, Deeks JJ, Demicheli V, Jefferson T (2010). Graves PM, ed. "Vaccines for preventing cholera: killed whole cell or other subunit vaccines (injected)". Cochrane Database Syst. Rev. (8): CD000974. doi:10.1002/14651858.CD000974.pub2. PMID 20687062.
^ "Cholera vaccines". Health topics. WHO. 2008. Archived from the original on 2010-02-16. Retrieved 2010-02-01.
^ ab Ramamurthy T (2010). Epidemiological and Molecular Aspects on Cholera. Springer. p. 330. ISBN 978-1-60327-265-0. Archived from the original on 2015-11-07.
^ ab Merrill RM (2010). Introduction to epidemiology (5th ed.). Sudbury, MA: Jones and Bartlett Publishers. p. 43. ISBN 978-0-7637-6622-1. Archived from the original on 2015-11-06.
^ Starr C (2007). Biology: Today and Tomorrow with Physiology (2 ed.). Cengage Learning. p. 563. ISBN 978-1-111-79701-0. Archived from the original on 2015-11-07.
^ ab THE TREATMENT OF DIARRHOEA, A manual for physicians and other senior health workers Archived 2011-10-19 at the Wayback Machine., World Health Organization, 2005. See page 10 (14 in PDF) and esp chapter 5; "MANAGEMENT OF SUSPECTED CHOLERA", pages 16–17 (20–21 in PDF).
^ "Community Health Worker Training Materials for Cholera Prevention and Control" (PDF). Centers for Disease Control and Prevention. Archived (PDF) from the original on 2017-07-02.
^ globalhealthcenter.umn.edu Archived 2013-12-03 at the Wayback Machine.
^ The Civil War That Killed Cholera Archived 2013-12-20 at the Wayback Machine., foreignpolicy.com.
^ 22nd April 2009: Sugary drinks worsen stomach 'bug'. BBC News, Health. citing National Institute for Health and Clinical Excellence. Seen 19th Dec. 2015 "Archived copy". Archived from the original on 2015-12-22. Retrieved 2015-12-18.CS1 maint: Archived copy as title (link)
^ "Oral Rehydration Solutions: Made at Home". The Mother and Child Health and Education Trust. 2010. Archived from the original on 2010-11-24. Retrieved 2010-10-29.
^ ab "First steps for managing an outbreak of acute diarrhea" (PDF). World Health Organization Global Task Force on Cholera Control. Archived (PDF) from the original on August 5, 2014. Retrieved November 23, 2013.
^ Cholera Treatment (Report). Centers for Disease Control and Prevention (CDC). November 28, 2011. Archived from the original on March 11, 2015.
^ "Cholera treatment". Molson Medical Informatics. 2007. Archived from the original on 6 November 2012. Retrieved 2008-01-03.
^ Krishna BV, Patil AB, Chandrasekhar MR (March 2006). "Fluoroquinolone-resistant Vibrio cholerae isolated during a cholera outbreak in India". Trans. R. Soc. Trop. Med. Hyg. 100 (3): 224–6. doi:10.1016/j.trstmh.2005.07.007. PMID 16246383.
^ ab Leibovici-Weissman, Y; Neuberger, A; Bitterman, R; Sinclair, D; Salam, MA; Paul, M (19 June 2014). "Antimicrobial drugs for treating cholera". Cochrane Database Syst. Rev. (6): CD008625. doi:10.1002/14651858.CD008625.pub2. PMC 4468928. PMID 24944120.
^ ab Cholera-Zinc Treatment (Report). Centers for Disease Control and Prevention (CDC). November 28, 2011. Archived from the original on December 3, 2013.
^ Telmesani AM (May 2010). "Oral rehydration salts, zinc supplement and rota virus vaccine in the management of childhood acute diarrhea". J. Fam. Community Med. 17 (2): 79–82. doi:10.4103/1319-1683.71988. PMC 3045093. PMID 21359029.
^ Todar K. "Vibrio cholerae and Asiatic Cholera". Todar's Online Textbook of Bacteriology. Archived from the original on 2010-12-28. Retrieved 2010-12-20.
^ Presenter: Richard Knox (10 December 2010). "NPR News". Morning Edition. NPR.
^ Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et al. (December 15, 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604.
^ Reidl J, Klose KE (June 2002). "Vibrio cholerae and cholera: out of the water and into the host". FEMS Microbiol. Rev. 26 (2): 125–39. doi:10.1111/j.1574-6976.2002.tb00605.x. PMID 12069878.
^ Johannes Bruwer (25 June 2017). "The horrors of Yemen's spiralling cholera crisis". BBC.
^ Dwyer, Colin. "Yemen Now Faces 'The Worst Cholera Outbreak In The World,' U.N. Says". National Public Radio. Retrieved 25 June 2017.
^ Blake PA (1993). "Epidemiology of cholera in the Americas". Gastroenterol. Clin. N. Am. 22 (3): 639–60. PMID 7691740.
^ ab Rosenberg, Charles E. (1987). The cholera years: the United States in 1832, 1849 and 1866. Chicago: University of Chicago Press. ISBN 978-0-226-72677-9.
^ "Cholera's seven pandemics Archived 2016-03-02 at the Wayback Machine.". CBC News. October 22, 2010.
^ Hays, JN (2005). Epidemics and Pandemics: Their Impacts on Human History. ABC-CLIO. p. 193. ISBN 978-1-85109-658-9.
^ McNeill, William H, Plagues and People, p. 268.
^ McNeil J. Something New Under The Sun: An Environmental History of the Twentieth Century World (The Global Century Series).
^ "Cholera – Vibrio cholerae infection | Cholera | CDC". www.cdc.gov. 2017-05-16. Retrieved 2018-04-04.
^ Aberth, John (2011). Plagues in World History. Lanham, MD: Rowman & Littlefield. p. 102. ISBN 978-0-7425-5705-5.
^ Kelley Lee (2003) "Health impacts of globalization: towards global governance". Palgrave Macmillan. p.131.
ISBN 0-333-80254-3
^ Geoffrey A. Hosking (2001). "Russia and the Russians: a history". Harvard University Press. p. 9.
ISBN 0-674-00473-6
^ Byrne JP (2008). Encyclopedia of Pestilence, Pandemics, and Plagues: A–M. ABC-CLIO. p. 99. ISBN 978-0-313-34102-1.
^ J. N. Hays (2005). "Epidemics and pandemics: their impacts on human history". p.347.
ISBN 1-85109-658-2
^ Sehdev PS (November 2002). "The origin of quarantine". Clin. Infect. Dis. 35 (9): 1071–2. doi:10.1086/344062. PMID 12398064.
^ Renbourn, E. T. (2012). "The History of the Flannel Binder and Cholera Belt". Med. Hist. 1 (3): 211–25. doi:10.1017/S0025727300021281. PMC 1034286. PMID 13440256.
^ www.legatum.sk Archived 2013-05-14 at the Wayback Machine., The American Homoeopathic Review Vol. 06 No. 11-12, 1866, pages 401–403
^ "Cholera Infantum, Tomatoes Will Relieve". October 13, 2008. Archived from the original on December 24, 2013.
^ "Cholera", World Health Organization. who.int Archived 2013-10-25 at the Wayback Machine.
^ Pyle GF (2010). "The Diffusion of Cholera in the United States in the Nineteenth Century". Geogr. Anal. 1: 59–75. doi:10.1111/j.1538-4632.1969.tb00605.x. PMID 11614509.
^ Lacey SW (1995). "Cholera: calamitous past, ominous future". Clin. Infect. Dis. 20 (5): 1409–19. doi:10.1093/clinids/20.5.1409. PMID 7620035.
^ Charles E. Rosenberg (2009). The Cholera Years the United States in 1832, 1849, and 1866. Chicago: University of Chicago Press. p. 74. ISBN 978-0-226-72676-2. Archived from the original on 2015-11-09.
^ See:
- Fillipo Pacini (1854) "Osservazioni microscopiche e deduzioni patologiche sul cholera asiatico" Archived 2015-11-18 at the Wayback Machine. (Microscopic observations and pathological deductions on Asiatic cholera), Gazzetta Medica Italiana: Toscana, 2nd series, 4 (50) : 397–401 ; 4 (51) : 405–412.
- Reprinted (more legibily) as a pamphlet. Archived 2015-11-10 at the Wayback Machine.
^ onlinelibrary.wiley.com Archived 2015-02-11 at the Wayback Machine.
^ haffkineinstitute.org Archived 2015-09-24 at the Wayback Machine.
^ Dr John Snow, The mode of communication of cholera Archived 2015-11-06 at the Wayback Machine., 2nd ed. (London, England: John Churchill, 1855).
^ Aberth, John. Plagues in World History. Lanham, MD: Rowman & Littlefield, 2011, 101.
^ "Albert Lasker Clinical Medical Research Award". Lasker Foundation. Archived from the original on September 1, 2017. Retrieved June 30, 2017.
^ Merrell DS, Butler SM, Qadri F, Dolganov NA, Alam A, Cohen MB, Calderwood SB, Schoolnik GK, Camilli A (June 2002). "Host-induced epidemic spread of the cholera bacterium". Nature. 417 (6889): 642–5. Bibcode:2002Natur.417..642M. doi:10.1038/nature00778. PMC 2776822. PMID 12050664.
^ "Cholera vaccines. A brief summary of the March 2010 position paper" (PDF). World Health Organization. Retrieved September 19, 2013.
^ Walton DA, Ivers LC (2011). "Responding to cholera in post-earthquake Haiti". N. Engl. J. Med. 364 (1): 3–5. doi:10.1056/NEJMp1012997. PMID 21142690.
^ Pauw J (2003). "The politics of underdevelopment: metered to death-how a water experiment caused riots and a cholera epidemic". Int. J. Health Serv. 33 (4): 819–30. doi:10.2190/kf8j-5nqd-xcyu-u8q7. PMID 14758861.
^ ab John TJ, Rajappan K, Arjunan KK (2004). "Communicable diseases monitored by disease surveillance in Kottayam district, Kerala state, India". Indian J. Med. Res. 120 (2): 86–93. PMID 15347857.
^ Siddique AK, Zaman K, Baqui AH, Akram K, Mutsuddy P, Eusof A, Haider K, Islam S, Sack RB (June 1992). "Cholera epidemics in Bangladesh: 1985–1991". J. Diarrhoeal Dis. Res. 10 (2): 79–86. PMID 1500643. Archived from the original on 2015-11-17.
^ DeRoeck D, Clemens JD, Nyamete A, Mahoney RT (2005). "Policymakers' views regarding the introduction of new-generation vaccines against typhoid fever, shigellosis and cholera in Asia". Vaccine. 23 (21): 2762–2774. doi:10.1016/j.vaccine.2004.11.044. PMID 15780724.
^ Choe, Chongwoo; Raschky, Paul A. (January 2016). "Media, institutions, and government action: prevention vs. palliation in the time of cholera". Eur. J. Political Econ. 41: 75–93. doi:10.1016/j.ejpoleco.2015.11.001.
^ Pruyt, Eric (26 July 2009). "Cholera in Zimbabwe" (PDF). Delft University of Technology. Archived from the original (PDF) on 20 October 2013.
^ ab Kapp C (February 2009). "Zimbabwe's humanitarian crisis worsens". Lancet. 373 (9662): 447. doi:10.1016/S0140-6736(09)60151-3. PMID 19205080. Archived from the original on 2009-08-27.
^ Brown, Man and Music, 430–32; Holden, 371; Warrack, Tchaikovsky, 269–270.
^ David Brown, Early Years, 46.
^ Holden, 23.
^ Brown, Man and Music, 431–35; Holden, 373–400.
^ Orata, Fabini; Keim, Paul S.; Boucher, Yan (April 2014). "The 2010 Cholera Outbreak in Haiti: How Science solved a Controversy". PLOS Pathog. 10 (4).
^ Asimov, Isaac (1982), Asimov's Biographical Encyclopedia of Science and Technology (2nd rev. ed.), Doubleday
^ Susan Nagel, Marie Thérèse: Child of Terror, p. 349-350.
^ Haynes SW (1997). James K. Polk and the Expansionist Impulse. New York: Longman. p. 191. ISBN 978-0-673-99001-3.
^ Smith, Rupert, The Utility of Force, Penguin Books, 2006, page 57
^ The Singapore Free Press and Mercantile Advertiser, 25 March 1893, Page 2 Archived 8 August 2014 at the Wayback Machine.
External links
| Classification | D
|
|---|---|
| External resources |
|
| Wikimedia Commons has media related to Cholera. |
| Look up Cholera in Wiktionary, the free dictionary. |
- Prevention and control of cholera outbreaks: WHO policy and recommendations
Cholera—World Health Organization
Cholera – Vibrio cholerae infection—Centers for Disease Control and Prevention
 "Cholera". Encyclopædia Britannica. 6 (11th ed.). 1911. pp. 262–267.
"Cholera". Encyclopædia Britannica. 6 (11th ed.). 1911. pp. 262–267.
 Cholera portal
Cholera portal